Injury epidemiology is the study of the distribution and determinants of injuries and safety-related events in populations, and the application of findings to prevent injuries or promote safety.
Transportation and Injury Studies
Rudisill, T. M. (2017). Fueled by an epidemic: a spatial analysis of opioid-positive drivers fatally injured in motor vehicle collisions in West Virginia, 2011-2015. American Journal of Public Health, 5(4), 124-129.
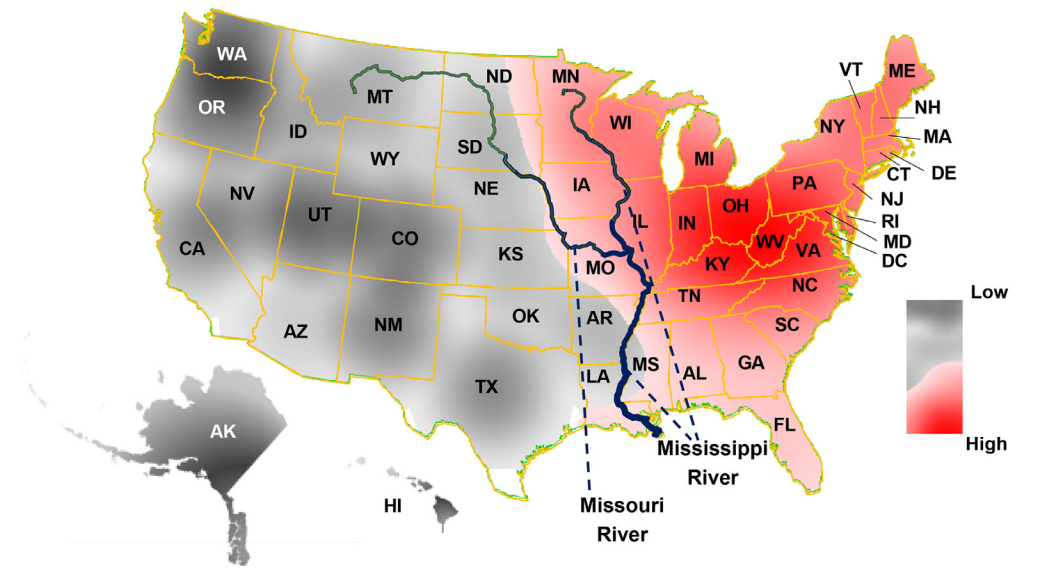
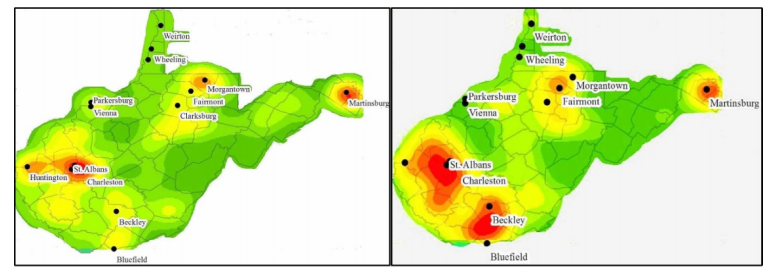
Background. Narcotics usage is associated with an increased risk of motor vehicle collision and opioid overdose deaths are elevated in West Virginia compared to other states in the United States. This analysis sought to determine the prevalence of narcotics among drivers fatally injured in motor vehicle collisions in West Virginia and to determine if these collisions were clustered in areas of the state where opioid use/abuse is high.
Methodology/Principal Findings. Fatal crash data from 2011-2015 were obtained from the Fatality Analysis Reporting System and the locations of the collisions were plotted with spatial software. Spatial analyses, including nearest neighbor indexes, heat maps and hot-spots, were conducted to determine if and where clusters of opioid-positive crashes existed. The results of the spatial analyses were visually compared to the rates of opioid overdose deaths by county, which served as a proxy of opioid use/abuse. Of the 486 drivers, 19% (n=94) tested positive for opioids. A clustering of opioid positive crashes was detected in the state overall (nearest neighbor index=0.89, p-value=0.055). Hot-spots were detected in the lower regions of the state, which overlapped counties with the highest rates of opioid overdose deaths, and cold-spots were detected in areas with lower opioid overdose death rates.
Conclusions/Significance. Individuals using narcotics may still operate motor vehicles, which may pose a threat to all road users in West Virginia. Public health interventions, education, or enforcement may be needed in areas of high opioid use/abuse to raise awareness of driving under the influence of drugs.
Rudisill, T. M., Menon, S., Hendricks, B., Zhu, M., & Smith, G. S. (2019). Differences between occupational and non-occupational-related motor vehicle collisions in West Virginia: A cross-sectional and spatial analysis. PLoS one, 14(12), e0227388.
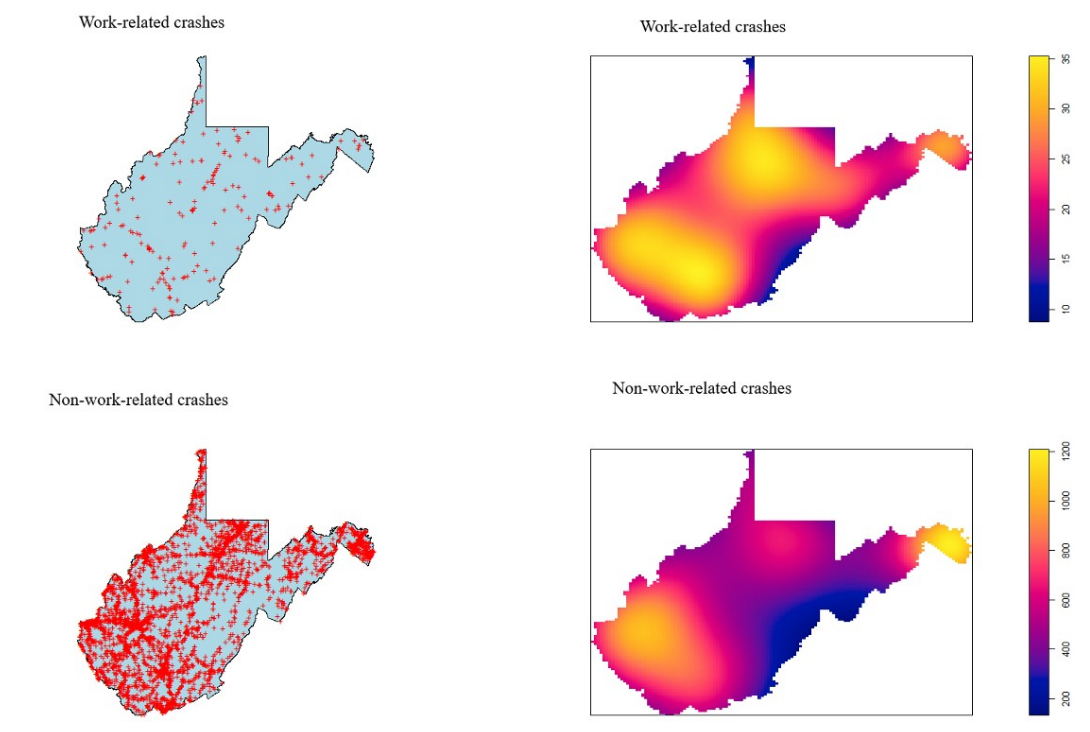
Background. Motor vehicle collisions comprise the majority of occupational-related fatalities in the United States and West Virginia has one of the highest occupational-related fatality rates in the nation. The purpose of this study was to compare work and non-work-related collisions, crash locations, and the characteristics of in-state and out-of-state drivers greater than or equal to 18 years of age who were fatally injured in work-related collisions in West Virginia.
Methodology. Data were from the 2000–2017 Fatality Analysis Reporting System. Work and non-work related crashes and characteristics in-state vs. out-of-state drivers were compared using binary and multivariable logistic regression analyses. Crash locations were compared via spatial analyses using kernel density estimations.
Results. Among the 5,835 individuals fatally injured in crashes, 209 were designated ‘at work’. The odds of being a work-related crash were 85% lower [Odds Ratio (OR) = 0.15; 95% confidence interval (CI): 0.04, 0.49] among those testing positive for alcohol, but 2.5 times greater (OR = 2.56; 95% CI: 1.16, 5.65) among those holding a commercial driver’s license. The odds of being an in-state driver were 75% lower (OR = 0.25; 95% CI: 0.12, 0.53) among those wearing a safety belt, but 2.7 times greater among workers testing drug positive (OR = 2.67; 95% CI: 1.10, 6.52). In-state drivers were also less likely to be driving a large truck or be involved in single vehicle collisions and less likely to experience crashes on weekends, nights, or on highways. Spatial patterns of crash locations varied slightly between workers and non-workers.
Conclusions. Work-related crashes differed greatly from non-work-related crashes in West Virginia. Stark differences existed between in-state and out-of-state workers and their crashes. Various avenues for workplace safety interventions exist, including seatbelt initiatives and drug testing policies for non-commercial drivers, which could help mitigate West Virginia’s elevated, occupational-related, traffic fatality rate.
Substance Abuse Epidemiology Studies
Dai, Zheng, Gordon S. Smith, Brian Hendricks, and Ruchi Bhandari. "Brief report: Cause of death among people discharged from infective endocarditis related hospitalization—West Virginia, 2016–2019." Clinical Cardiology 45, no. 5 (2022): 536-539.
Background and Objectives
Compare proportion of all-cause and cause-specific mortality among West Virginia Medicaid enrollees who were discharged from infective endocarditis (IE) hospitalization with and without opioid use disorder (OUD) diagnosis.
Methods
The proportions of cause-specific deaths among those who were discharged from IE-related hospitalizations were compared by OUD diagnosis.
Results
The top three underlying causes of death discharged from IE hospitalization were accidental drug poisoning, mental and behavioral disorders due to polysubstance use, and cardiovascular diseases. Of the total deaths occurring among patients discharged after IE-related hospitalization, the proportion has increased seven times from 2016 to 2019 among the OUD deaths while it doubled among the non-OUD deaths.
Discussion and Conclusions
Of the total deaths occurring among patients discharged after IE-related hospitalization, the increase is higher in those with OUD diagnosis. OUD is becoming a significantly negative impactor on the survival outcome among IE patients. It is of growing importance to deliver medication for OUD treatment and harm reduction efforts to IE patients in a timely manner, especially as the COVID-19 pandemic persists.
Allen, Lindsay, Nathan Pauly, Zheng Dai, Rebecca Wallis, Brian Hendricks, and Thomas Bias. "Drive Times to Methadone Treatment among Medicaid Patients." Journal of Health Care for the Poor and Underserved 33, no. 3 (2022): 1169-1176.
Objective
To describe round-trip drive times and travel distance to methadone clinics among Medicaid enrollees in West Virginia, testing for differences between those in
rural versus urban areas.
Findings
In this cross-sectional analysis of West Virginia Medicaid enrollees’ claims from 2018–2019, methadone recipients on average traveled almost an hour round-trip to receive their daily treatment. The travel burden was substantially higher among those in more rural areas.
Meaning
These findings indicate that it may be difficult for patients to adhere to their methadone treatment regimen, perhaps leading to suboptimal treatment rates and outcomes.
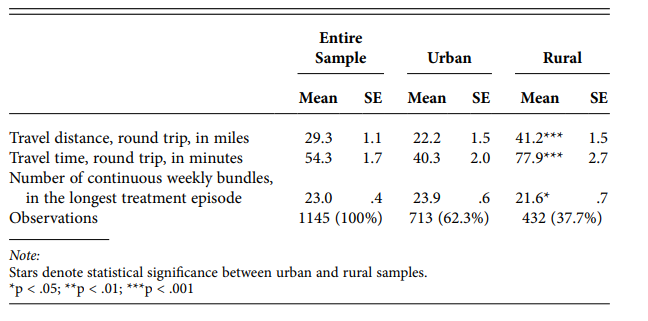
MEDICAID ENROLLEES, 2018–2019, BY RURAL STATUS
Haggerty, Treah, Maryam Khodaverdi, Patricia Dekeseredy, Nathan Wood, Brian Hendricks, Jason Peklinsky, and Cara L. Sedney. "Assessing the impact of social distancing measures implemented during COVID-19 pandemic on medications for opioid use disorder in West Virginia." Journal of Substance Abuse Treatment 136 (2022): 108687.
Introduction
This study evaluates if social distancing measures instituted during the novel coronavirus SARS-CoV-2 (COVID-19) pandemic were associated with a reduction in Medication for Opioid Use Disorder (MOUD) prescribing in West Virginia. The COVID-19 pandemic necessitated the quick implementation of public health interventions such as social distancing. This led to the use of telemedicine in the clinical setting however implementing telemedicine involves system level and infrastructure level changes within a healthcare environment. This could cause a barrier to MOUD delivery as it is often provided concomitantly with other face to face substance use and mental health services. The purpose of this study is to determine whether social distancing was associated with a reduction in MOUD prescribing in West Virginia, with the goal of adding to the knowledge of how COVID-19 and COVID-19-related mitigation strategies have impacted patients with OUD.
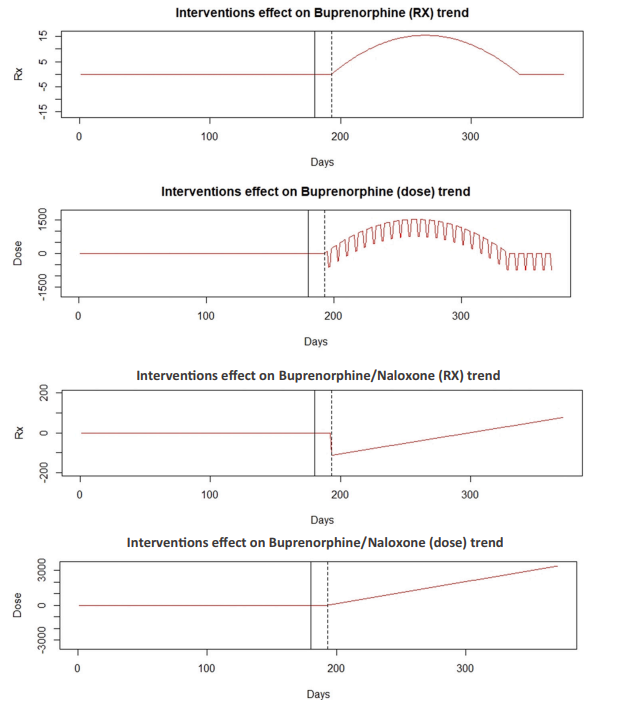
Methods
Prescription monitoring data were requested from the West Virginia Board of Pharmacy. We applied interrupted time series modeling to investigate MOUD prescribing practices before and after social distancing took effect. Gabapentin prescriptions were utilized as a control for comparison.
Results
Our study assessed state-wide buprenorphine and Suboxone prescriptions as compared to a control medication and found an increase in dosage of both medications and an increase in number of buprenorphine prescriptions, but a small decrease in buprenorphine/naloxone prescription number related to the dates of implementation of social distancing. Taken together, overall this indicates an increase in prescription number of MOUD prescriptions as well as an increase in dosage.
Conclusion
This study suggests that social distancing measures were associated with an increase in both the number of MOUD prescriptions and the number of doses in each prescription. Significant alterations to MOUD delivery in the clinical setting were implemented in a short timeframe with the COVID-19 pandemic. Understanding the implementation of clinical measures to accommodate social distancing measures may provide benefit to transformation of future delivery of MOUD.
Hendricks, Brian, George Sokos, Wes Kimble, Zheng Dai, Olayemi Adeniran, Mohammed Osman, Gordon Stephen Smith, and Chris Bianco. "Clinical and demographic factors associated with stimulant use disorder in a rural heart failure population." Drug and Alcohol Dependence 229 (2021): 109060.
Background: Heart failure is becoming increasingly common among patients under 50 years of age, particularly in African Americans and patients with stimulant use disorder. Yet the sources of these disparities remain poorly understood. This study identified key demographic and clinical factors associated with stimulant use disorder in a largely rural heart failure patient registry.
Methods: Patient records reporting a diagnosis of heart failure between January 2008 and March 2020 were requested from West Virginia University Hospital Systems (n=37,872). Odds of stimulant use disorder were estimated by demographic group (age, race, sex), insurance carrier, and clinical comorbidities using logistic regression.
Results: Multivariable regression analysis identified higher odds of stimulant use disorder among Black/African Americans (1.95 [1.32, 2.77]) and patients who report drinking one or more alcoholic drinks per week (2.23 [1.72, 2.88]). Lower odds of stimulant use disorder were identified among patients with hypertension (0.59 [0.47, 0.73]), or diabetes (0.65 [0.52, 0.81]).. Likewise, lower odds of stimulant use disorder were noted among females, patients older than 30 years of age and those not enrolled in Medicaid.
Conclusion: These results highlight the alarming extent to which Medicaid enrollees, Black/African Americans, people aged 18–24 and 25–44, or persons with a past alcohol use disorder diagnosis are associated with stimulant use disorder among heart failure populations living in largely rural areas. Additionally, they emphasize the need to develop policies and refine clinical care that affects this vulnerable population’s prognoses.
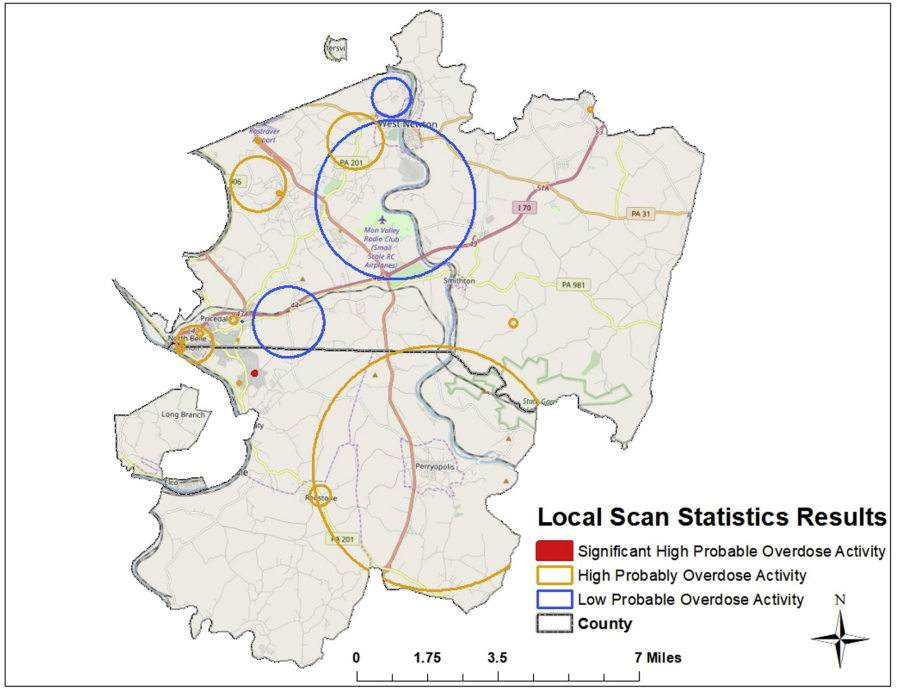
Pesarsick, J., Gwilliam, M., Adeniran, O., Rudisill, T., Smith, G., & Hendricks, B. (2019). Identifying high-risk areas for nonfatal opioid overdose: a spatial case-control study using EMS run data. Annals of epidemiology, 36, 20-25.
Purpose. The objective of our study was to incorporate stricter probable nonfatal opioid overdose case criteria, and advanced epidemiologic approaches to more reliably detect local clustering in nonfatal opioid overdose activity in EMS runs data.
Methods. Data were obtained using emsCharts for our study area in southwestern Pennsylvania from 2007 to 2018. Cases were identified as emergency medical service (EMS) responses where naloxone was administered, and improvement was noted in patient records between initial and final Glasgow Coma Score. A subsample of all-cause EMS responses sites were used as controls and exact matched to cases on sex and 10-year-age category. Clustering was assessed using difference in Ripley's K function for cases and controls and Kulldorff scan statistics.
Results. Difference in K functions indicated no significant difference in probable nonfatal overdose EMS runs across the study area compared to all-cause EMS runs. However, scan statistics did identify significant local clustering of probable nonfatal overdose EMS runs (maximum likelihood = 16.40, P = 0.0003).
Conclusions. Results highlight relevance of EMS data to detect community-level overdose activity and promote reliable use through stricter case definition criteria and advanced methodological approaches. Techniques examined have the potential to improve targeted delivery of neighborhood-level public health response activities using a near real-time data source.
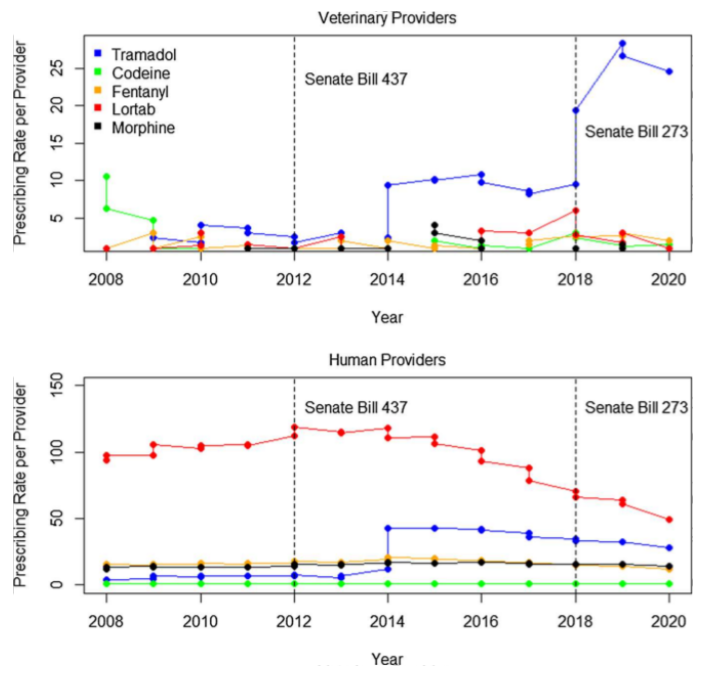
Hendricks, B., Rudisill, T., Pesarsick, J., Wen, S., Dotson, T., Wood, N., & Smith, G. S. (2021). Prescription drug monitoring program policy reform: human and veterinary practitioner prescribing in West Virginia, 2008–2020. Journal of Public Health Policy, 1-9.
Background. No study has examined Prescription Drug Monitoring Program (PDMP) data for West Virginia or among specialty practices, such as veterinary medicine. The objectives of this study were to conduct time series modeling to describe the PDMP policy reform impact on prescribing rates for human and veterinary providers.
Methods. We obtained data from the WV PDMP for 2008 through 2020 for the number of opioid prescriptions filled and providers. We estimated prescribing rates for human and veterinary providers separately based upon the top five opioids prescribed by veterinarians. We estimated temporal effects using a Bayesian log-normal time series model for humans and veterinarians separately.
Findings. Throughout the study period prescribing rates increased significantly for veterinarians, and decreased for human providers, particularly during 2018 after implementation of the Opioid Reduction Act. Findings provide novel insight into the differential impact of policy on specialty practices and highlight decreasing human opioid prescribing observed elsewhere.
Mental Health and Injury Studies
Rockett, Ian RH, Haomiao Jia, Bina Ali, Aniruddha Banerjee, Hilary S. Connery, Kurt B. Nolte, Ted Miller et al. "Association of state social and environmental factors with rates of self-injury mortality and suicide in the United States." JAMA network open 5, no. 2 (2022): e2146591-e2146591.
IMPORTANCE
Self-injury mortality (SIM) combines suicides and the preponderance of drug misuse–related overdose fatalities. Identifying social and environmental factors associated with SIM and
suicide may inform etiologic understanding and intervention design.
OBJECTIVE
To identify factors associated with interstate SIM and suicide rate variation and to assess potential for differential suicide misclassification.
DESIGN, SETTING, AND PARTICIPANTS
This cross-sectional study used a partial panel time series
with underlying cause-of-death data from 50 US states and the District of Columbia for 1999-2000,
2007-2008, 2013-2014 and 2018-2019. Applying data from the Centers for Disease Control and
Prevention, SIM includes all suicides and the preponderance of unintentional and undetermined drug
intoxication deaths, reflecting self-harm behaviors. Data were analyzed from February to June 2021.
EXPOSURES
Exposures included inequity, isolation, demographic characteristics, injury mechanism, health care access, and medicolegal death investigation system type.
MAIN OUTCOMES AND MEASURES
The main outcome, SIM, was assessed using unstandardized regression coefficients of interstate variation associations, identified by the least absolute shrinkage
and selection operator; ratios of crude SIM to suicide rates per 100 000 population were assessed for potential differential suicide misclassification.
RESULTS
A total of 101 325 SIMs were identified, including 74 506 (73.5%) among males and 26 819 (26.5%) among females. SIM to suicide rate ratios trended upwards, with an accelerating increase in overdose fatalities classified as unintentional or undetermined (SIM to suicide rate ratio, 1999-2000: 1.39; 95% CI, 1.38-1.41; 2018-2019: 2.12; 95% CI, 2.11-2.14). Eight states recorded a SIM to suicide rate ratio less than 1.50 in 2018-2019 vs 39 states in 1999-2000. Northeastern states concentrated in the highest category (range, 2.10-6.00); only the West remained unrepresented. Least absolute shrinkage and selection operator identified 8 factors associated with the SIM rate in 2018-2019: centralized medical examiner system (β = 4.362), labor underutilization rate (β = 0.728), manufacturing employment (β = −0.056), homelessness rate (β = −0.125), percentage nonreligious (β = 0.041), non-Hispanic White race and ethnicity (β = 0.087), prescribed opioids for 30 days or more (β = 0.117), and percentage without health insurance (β = −0.013) and 5 factors associated with the suicide rate: percentage male (β = 1.046), military veteran (β = 0.747), rural (β = 0.031), firearm ownership (β = 0.030), and pain reliever misuse (β = 1.131).
CONCLUSIONS AND RELEVANCE
These findings suggest that SIM rates were associated with modifiable, upstream factors. Although embedded in SIM, suicide unexpectedly deviated in
Rockett, I. R., Caine, E. D., Banerjee, A., Ali, B., Miller, T., Connery, H. S., ... & Jia, H. (2021). Fatal self-injury in the United States, 1999–2018: Unmasking a national mental health crisis. EClinicalMedicine, 32, 100741.
Background. Suicides by any method, plus ‘nonsuicide’ fatalities from drug self-intoxication (estimated from selected forensically undetermined and ‘accidental’ deaths), together represent self-injury mortality (SIM)— fatalities due to mental disorders or distress. SIM is especially important to examine given frequent undercounting of suicides amongst drug overdose deaths. We report suicide and SIM trends in the United States of America (US) during 1999 to 2018, portray interstate rate trends, and examine spatiotemporal (spacetime) diffusion or spread of the drug self-intoxication component of SIM, with attention to potential for differential suicide misclassification.
Methods. For this state-based, cross-sectional, panel time series, we used de-identified manner and underlying cause-of-death data for the 50 states and District of Columbia (DC) from CDC’s Wide-ranging Online Data for Epidemiologic Research. Procedures comprised joinpoint regression to describe national trends; Spearman’s rank order correlation coefficient to assess interstate SIM and suicide rate congruence; and spacetime hierarchical modelling of the ‘nonsuicide’ SIM component.
Findings. The national annual average percentage change over the observation period in the SIM rate was 4.3% (95% CI: 3.3%, 5.4%; p<0.001) versus 1.8% (95% CI: 1.6%, 2.0%; p<0.001) for the suicide rate. By 2017/ 2018, all states except Nebraska (19.9) posted a SIM rate of at least 21.0 deaths per 100,000 population—the floor of the rate range for the top 5 ranking states in 1999/2000. The rank-order correlation coefficient for SIM and suicide rates was 0.82 (p<0.001) in 1999/2000 versus 0.34 (p = 0.02) by 2017/2018. Seven states in the West posted a 5.0% reduction in their standardised mortality ratios of ‘nonsuicide’ drug fatalities, relative to the national ratio, and 6 states from the other 3 major regions a >6.0% increase (p<0.05).
Interpretation. Depiction of rising SIM trends across states and major regions unmasks a burgeoning national mental health crisis. Geographic variation is plausibly a partial product of local heterogeneity in toxic drug availability and the quality of medicolegal death investigations. Like COVID-19, the nation will only be able to prevent SIM by responding with collective, comprehensive, systemic approaches. Injury surveillance and prevention, mental health, and societal well-being are poorly served by the continuing segregation of substance use disorders from other mental disorders in clinical medicine and public health practice.