Cardiovascular disease epidemiology is the study of the distribution and determinants of health affecting the heart or blood vessels, with an intent to prevent or manage coronary heart disease, cerebrovascular disease, peripheral artery disease and more.
Cardiovascular Disease
Witrick, Brian, Corey A. Kalbaugh, Lu Shi, Rachel Mayo, and Brian Hendricks. "Geographic Disparities in Readmissions for Peripheral Artery Disease in South Carolina." International journal of environmental research and public health 19, no. 1 (2021): 285.
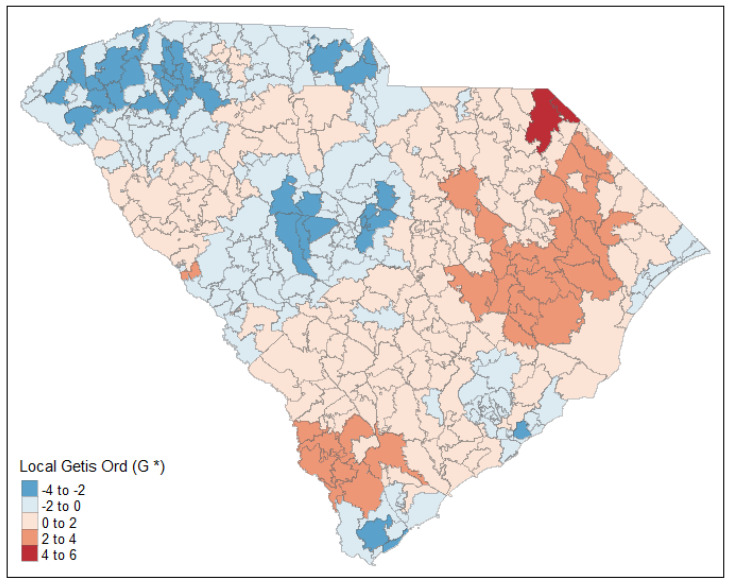
Readmissions constitute a major health care burden among peripheral artery disease (PAD) patients. This study aimed to 1) estimate the zip code tabulation area (ZCTA)-level prevalence of readmission among PAD patients and characterize the effect of covariates on readmissions; and (2) identify hotspots of PAD based on estimated prevalence of readmission. Thirty-day readmissions among PAD patients were identified from the South Carolina Revenue and Fiscal Affairs Office All Payers Database (2010–2018). Bayesian spatial hierarchical modeling was conducted to identify areas of high risk, while controlling for confounders. We mapped the estimated readmission rates and identified hotspots using local Getis Ord (G*) statistics. Of the 232,731 individuals admitted to a hospital or outpatient surgery facility with PAD diagnosis, 30,366 (13.1%) experienced an unplanned readmission to a hospital within 30 days. Fitted readmission rates ranged from 35.3 per 1000 patients to 370.7 per 1000 patients and the risk of having a readmission was significantly associated with the percentage of patients who are 65 and older (0.992, 95%CI: 0.985–0.999), have Medicare insurance (1.013, 1.005–1.020), and have hypertension (1.014, 1.005–1.023). Geographic analysis found significant variation in readmission rates across the state and identified priority areas for targeted interventions to reduce readmissions.
Minc, S. D., Hendricks, B., Misra, R., Ren, Y., Thibault, D., Marone, L., & Smith, G. S. (2020). Geographic variation in amputation rates among patients with diabetes and/or peripheral arterial disease in the rural state of West Virginia identifies areas for improved care. Journal of vascular surgery, 71(5), 1708-1717.
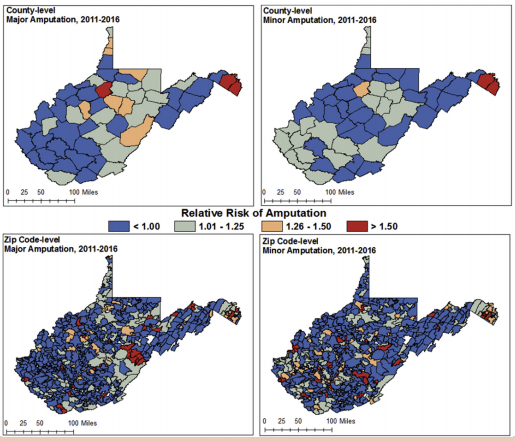
Objective. Amputation is a devastating but preventable complication of diabetes and peripheral arterial disease (PAD). Multiple studies have focused on disparities in amputation rates based on race and socioeconomic status, but few focus on amputation trends in rural populations. The objective of this study was to identify the prevalence of major and minor amputation among patients admitted with diabetes and/or PAD in a rural, Appalachian state, and to identify geographic areas with higher than expected major and minor amputations using advanced spatial analysis while controlling for comorbidities and rurality.
Methods. Patient hospital admissions of West Virginia residents with diagnoses of diabetes and/or PAD and with or without an amputation procedure were identified from the West Virginia Health Care Authority State Inpatient Database from 2011 to 2016 using relevant International Classification of Diseases, 9th edition and 10the edition codes. Bayesian spatial hierarchical modeling was conducted to identify areas of high risk, while controlling for important confounders for amputation.
Results. Overall, there were 5557 amputations among 459,452 hospital admissions with diabetes and/or PAD from 2011 to 2016. The majority of the amputations were minor (61.7%; n = 3430), with a prevalence of 7.5 per 1000 and 40.4% (n = 2248) were major, with a prevalence of 4.9 per 1000. Geographic analysis found significant variation in risk for both major and minor amputation across the state, even after adjusting for the prevalence of risk factors. Analyses indicated an increased risk of amputation in the central and northeastern regions of West Virginia at the county level, although zip code-level patterns of amputation varied, with high-risk areas identified primarily in the northeastern and south-central regions of the state.
Conclusions. There is significant geographic variation in risk of amputation across West Virginia, even after adjusting for disease-related risk factors, suggesting priority areas for further investigation. The level of granularity obtained using advanced spatial analyses rather than traditional methods demonstrate the value of this approach, particularly when risk estimates are used to inform policy or public health intervention.
Urology Studies
Ferari, Christopher, Katharina Mitchell, Chad Crigger, Shirley Zupper, Amy Wildasin, Michael Ost, Brian Hendricks, and Osama Al-Omar. "Bridging the Gap—Building Surgical Subspecialty Telemedicine Clinics in the Rural Setting." Urology Practice 9, no. 2 (2022): 126-133.
Introduction
Pediatric urology is a much-needed subspecialty with a breadth of complex disorders that can often prove challenging to diagnose and manage. Exacerbating this need is the minimal exposure medical trainees receive to pediatric urology. Pediatric urology arrived in West Virginia in 1983 but the subspecialty has been inconsistently represented since then. Currently there are 2 fellowship-trained pediatric urologists in the state of West Virginia, which has an area of approximately 24,038 square miles. We review our experience with the use of telemedicine in providing outreach to the wider parts of our medically underserved state and ultimately evaluate its efficacy from a patient-centric cost analysis and diagnosis concordance perspective. We hypothesized that the use of telemedicine would be cost and time-effective for patients in our rural state.
Methods
We retrospectively reviewed our series of patients presenting from outside telemedicine “referral centers” in Martinsburg, Parkersburg and Wheeling for pediatric urological consultation. We evaluated reason for consultation, geographic driving distance, drive time and travel cost saved from telemedicine consultation.
Results
A total of 92 patients presented to outside designated telemedicine centers from August 2018 to April 2020. The mean driving time saved utilizing telemedicine consultation was 4 hours and 46 minutes, and mean driving distance saved was 299.8 miles. Travel costs saved in terms of fuel averaged $173.88 per patient. The most common reason for consultation was undescended testis, followed by recurrent urinary tract infection and nocturnal enuresis. Of the 23 patients who required surgery, only 2 (8.7%) had an initial diagnosis that was not concordant with their operating room examination.
Conclusions
While modest, our data indicate a modern solution to a historical need in our state. Our high diagnosis concordance rate (91.3%) shows that a well-trained advanced practice provider can adequately perform an operative evaluation via telemedicine.